Parast Lab
- About
- Projects
- People
- Events
- Publications
Located at the Sanford Consortium for Regenerative Medicine, our laboratory is interested in the development and function of the placenta, a unique transient organ essential for proper fetal growth and development. The epithelial portion of the placenta is made of cells called "trophoblast" (from the Greek work meaning "to feed"). These cells are derived from trophectoderm, the outer layer of the early embryo, which differentiates into multiple subtypes of trophoblast, with different characteristics and function. Villous trophoblast, including cytotrophoblast and syncytiotrophoblast, serve to exchange gases and nutrients, while extravillous trophoblast invade maternal decidua and spiral arterioles and establish a blood supply for the growing placenta and fetus. Alterations in trophoblast differentiation and function lead to placental disease, and to various obstetric diseases and complications, including miscarriage, pre-eclampsia, fetal growth restriction, preterm birth, and stillbirth. Using mouse models, pluripotent stem cells, as well as primary human trophoblast cultures and placental explants and tissues, we are exploring the role of several transcription factors and signaling pathways involved in trophoblast differentiation and placental development. As part of the Center for Perinatal Discovery, our group is also involved in clinical and translational research projects, in which we evaluate the relationship between placental pathology and complications of pregnancy.
Learn more specific projects below:
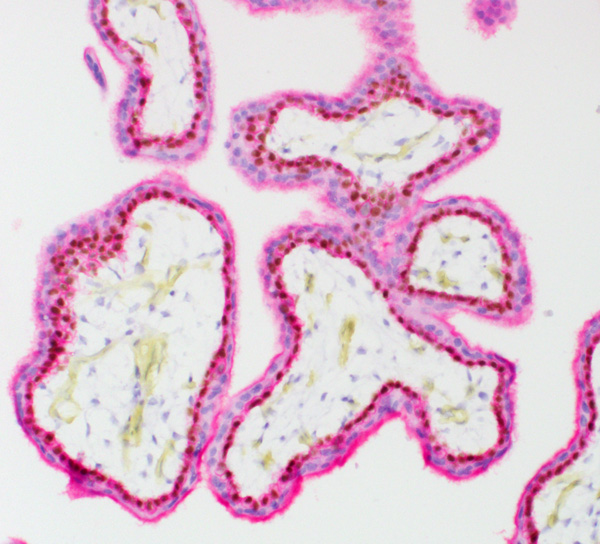
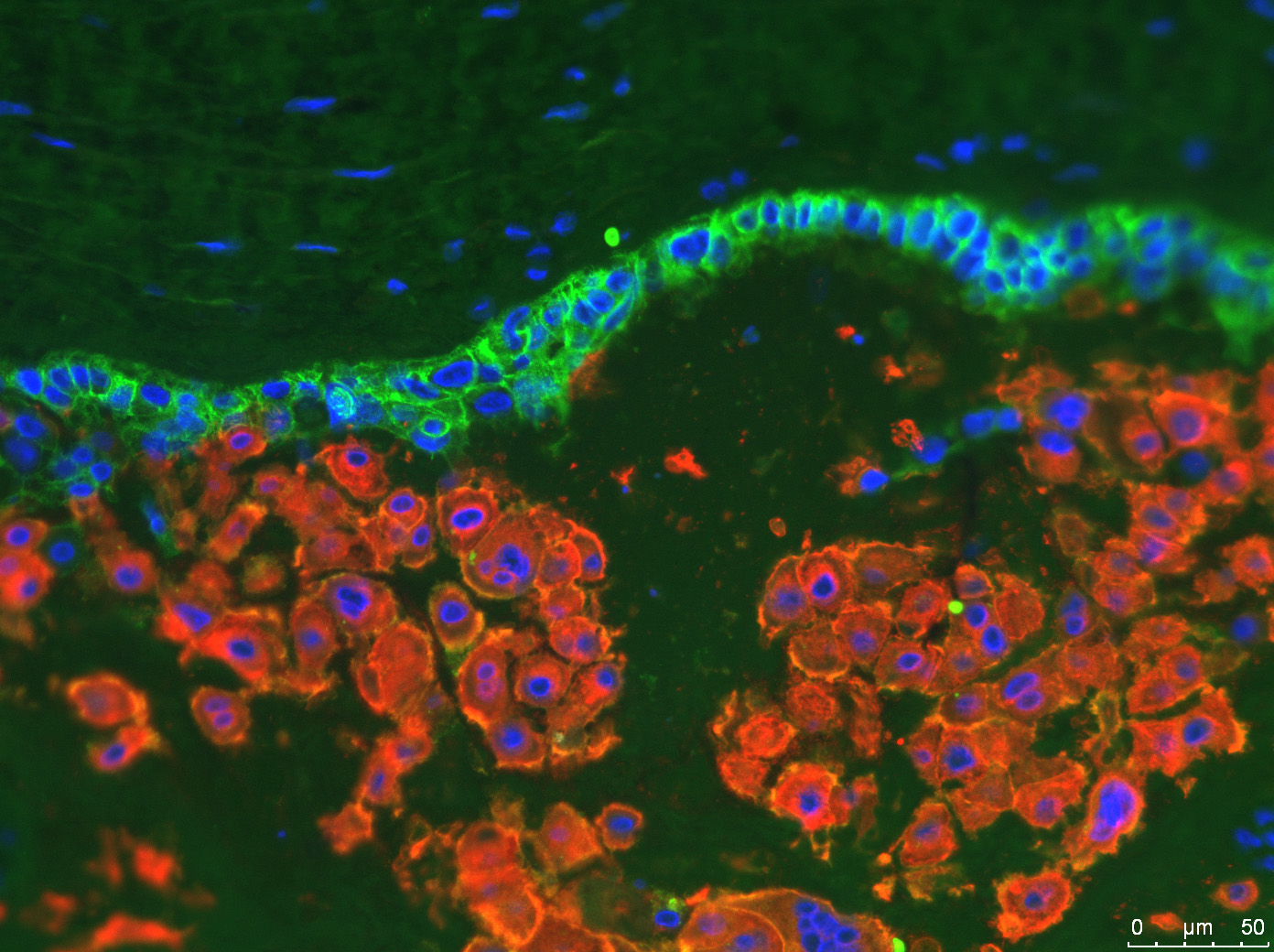
Unlike the mouse placenta, the human placental barrier is organized into a stratified epithelium, where the basal layer, the layer closest to the basement membrane of the chorionic villus, is comprised of cytotrophoblast (CTB) stem cells, which uniformly express the transcription factor p63. p63 is common to stem cells of other stratified epithelia, including skin and cervix, where it serves a dual role for maintenance of the stem cell state as well as initiation of differentiation. While its role in the placenta is less well-understood, our group has found that p63 is exclusively expressed in the CTB stem cells in the placenta and is excluded from more differentiated syncytiotrophoblast (STB) and extravillous trophoblast (EVT). In addition, while the CTB layer becomes discontinuous with increasing gestational age, p63 expression appears to be maintained in these cells. We are now using human primary trophoblast stem cells (TSC) to identify the role of p63 in CTB maintenance and differentiation. Finally, we have also identified other markers of the CTB stem cell state, and are applying single cell RNA sequencing to explore the heterogeneity of these cells in the human placenta. Understanding how CTB regulate proliferation vs. differentiation will help us to identify ways to target the placenta and promote its regeneration in the setting of placental dysfunction (including preeclampsia and fetal growth restriction).
The bulk of early placental development occurs under low oxygen conditions (2-8% oxygen); however, most tissue culture is conducted under atmospheric oxygen (21% oxygen). Studies in rodents (both mouse and rat) have shown that the transcription factor hypoxia-inducible factor (HIF) plays a significant role in placental development: in fact, without individual components of HIF, mouse embryos do not survive beyond mid-gestation due to abnormalities in the placenta. In fact, HIF plays a major role in differentiation of trophoblast giant cells, cells in the rodent placenta which are equivalent to the invasive extravillous trophoblast (EVT) in the human placenta. Our group has shown that, similar to rodents, human EVT also require an intact HIF complex for proper differentiation. We are now exploring the mechanisms through which hypoxia, and other related signaling pathways, induce both differentiation and maturation of EVT. To do this, we use an XVIVO Hypoxia Workstation (Biospherix) to conduct cell culture (including continuous passaging) under low oxygen conditions. Probing mechanisms of EVT differentiation is key to understanding early placental development, but also the pathophysiology of placental dysfunction (i.e. in the setting of miscarriage, preeclampsia, and fetal growth restriction), which are associated with hypoxia and abnormal EVT development.

Pluripotent stem cells (PSC's) are, by definition, able to contribute to all embryonic germ layers (endoderm, mesoderm, and ectoderm), but not to extraembryonic tissues (including placenta and trophoblast). However, as has now been shown by multiple groups, under specific culture conditions, the addition of bone morphogenetic protein-4 (BMP4) to human pluripotent stem cells (including embryonic stem cells/ESC and induced pluripotent stem cells/iPSC) induces the trophoblast lineage. Our group, in collaboration with Dr. Mariko Horii's, has established optimized protocols for trophoblast differentiation of hPSCs, and has taken advantage of this system to identify mechanisms of trophoblast lineage specification and model human trophoblast under both normal and diseased conditions. Our group has also identified a role for autocrine BMP signaling in trophoblast stem cells (TSC's). We are currently exploring the underlying mechanisms downstream of BMP signaling in trophoblast lineage specification and trophoblast stem cell maintenance, using both mouse and human PSC's and TSC's.

In collaboration with the Departments of Obstetrics, Gynecology, and Reproductive Sciences, and Pediatrics, our group is involved in multiple projects, in order to evaluate the link between placental pathology and complications of pregnancy, ranging from preeclampsia and fetal growth restriction, to gestational diabetes and macrosomia, to placenta accreta spectrum and pregnancy loss. These projects often involve an interdisciplinary group of researchers, from across the training spectrum (including undergraduate students, medical students, residents and clinical fellows), with the goal of advancing care for our patients.
Our lab is located at the Sanford Consortium for Regenerative Medicine, where visitors are always welcome.
Our group is highly collaborative, working with multiple other labs both within and outside the Department and UC San Diego to identify causes of pregnancy complications and pregnancy loss. If you are interested in joining the lab, please send a cover letter and CV to Dr. Parast: mparast@health.ucsd.edu.
Donations will advance research into pathophysiology and therapeutic targeting of placental disorders, including preeclampsia, fetal growth restriction, and stillbirth.